RELATED: Five things you didn’t know about pharmacy-benefit managers
The company said in a statement that it will be
- Limiting to seven days the supply of opioids dispensed for certain acute prescriptions.
- Limiting the daily dosage of opioids dispensed based on the strength of the opioid.
- Requiring the use of immediate-release formulations of opioids before extended-release opioids are dispensed.
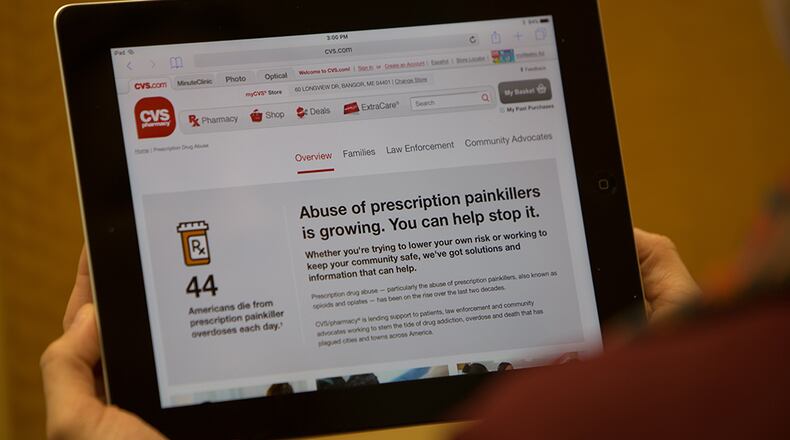
CVS Health Corp., the parent of CVS Caremark and the CVS retail pharmacy chain, also said it will have efforts to properly dispose of unused prescription medication, will have its pharmacists educate patients on opioid risks, and will continue to have its foundation donate to community health centers that have medication-assisted treatment and other addiction services.
RELATED: Local small pharmacies are disappearing, Medicaid cuts seen as culprit
RELATED: Drug discounts may contain catch
About the Author